An Overview of this Guide
This guide is intended to explain everything you need to know about Remote Patient Monitoring (RPM), including:
- An Introduction to RPM
- The Benefits of RPM
- How RPM Expands the Potential of Telehealth
- RPM Reimbursements & How They Work
- Tips for Facilitating CMS Compliance in Your Practice
- Getting Started with RPM
- How to Get the Most Out of Your RPM System
- How to Maximize Outcomes
- Common RPM Mistakes and How to Avoid Them
New Developments: Remote Therapeutic Monitoring
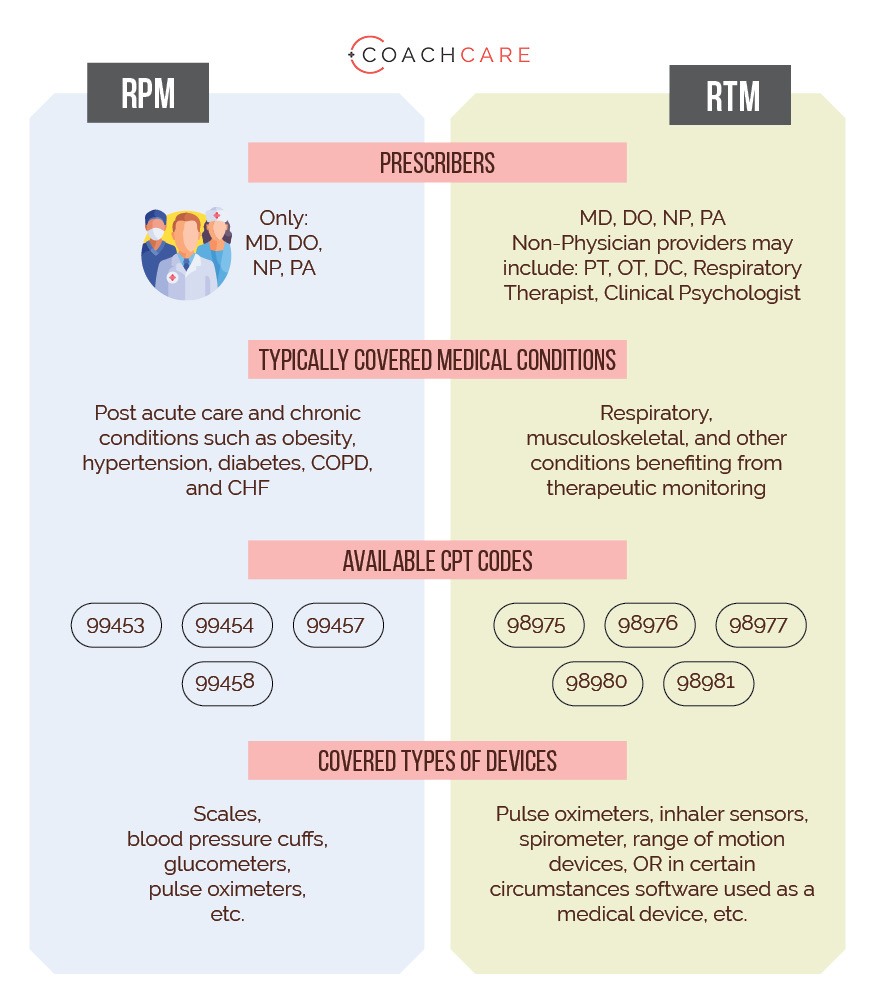
Recently, additional reimbursement has been approved for related services provided by chiropractors, physical therapists and certain other providers focused on musculo-skelatal conditions. This reimbursable protocol is referred to as Remote Therapeutic Monitoring (RTM). For your benefit, included below is a comparison chart between RPM and RTM. [For information about RTM, please click here.]
Section 1: An Introduction to RPM
Recently, a new treatment service, Remote Patient Monitoring, has experienced dramatic acceptance within the medical community for two primary reasons:
- Improved preventative, acute, and chronic care
- Significant financial benefit to providers
Care of patients outside the physical practice or hospital has been expanding for many years, particularly in the context of telehealth, conducting consultations with patients over the phone or using video tools. In the past two years, the use of telehealth has expanded dramatically since COVID-19 has made it very difficult, or even impossible, to see patients in person.
New technologies have made it possible for providers to monitor their patients’ vital signs and other medical information in real-time and from a distance. Software, particularly mobile apps, has been developed to interface directly with Bluetooth and wifi-enabled devices such as smart scales, blood pressure cuffs, glucometers, and pulse oximeters.
The population of the United States has been getting sicker. The prevalence of obesity has increased from 30% to 40% over the past two decades. In the United States, more than 34 million people suffer from diabetes and 47% from hypertension.
Given innovations in technology, new coverage for monitoring patients, the need to reduce the progression into, or the progression of existing, chronic conditions, Remote Patient Monitoring has become a well recognized component of patient care.
Section 2: The Benefits of Remote Patient Monitoring
Patients with chronic conditions and compromised health are at a greater risk for severe symptoms when they have other illnesses or injuries. The COVID-19 pandemic exposed the vulnerability caused by chronic health conditions and challenged medical practices to find better ways to help patients. Remote healthcare monitoring solutions offer an option with impressive benefits for doctors, patients, and our healthcare system as a whole.
Increasing Revenue & Profitability
Patients with chronic health conditions may be eager to use home health monitoring devices and services. Many people are looking for ways to receive medical care through telehealth options because of the risks associated with COVID-19 and the convenience of telehealth options. Patients who might otherwise skip office visits can now consult with you from their own home.
Remote Patient Monitoring can increase revenue and profitability in a number of ways.
- Reimbursement for RPM codes that can be over $200 per patient per month
- An increase in the number of consults you complete with existing patients
- An increase in the capacity of your practice through efficiencies
Making Better Use of Staff Time
Remote Patient Monitoring drives significant efficiency for practices and staff time. All tasks related to Remote Monitoring are completed by junior level staff, including medical assistants, licensed vocational nurses or front office staff (if entrusted with patient care). In particular, RPM frees up nurse schedules and has no impact on physician schedules. In addition, Remote Patient Monitoring systems often include automated alerts and escalation functionality that allows the entire practice to quickly triage patients and focus their time on those in need of an intervention.
Decreasing Hospital Admissions
When patients can’t or won’t come to see you in your office, they turn to urgent care centers and hospitals for emergency treatment. Remote healthcare monitoring systems help decrease hospitalizations by empowering your patients to take control of their health. Instead of waiting until a chronic health condition becomes an emergency, you can intervene proactively and your patients can seek help from the comfort of their own homes.
As it relates to reducing emergency room visits and the associated costs, medical practices experienced the following benefits after adding a remote health monitoring system, according to a recent study completed by the Mayo Clinic:
- 79% Greater patient involvement
- 6% fewer hospitalizations among patients
- 29% fewer emergency room visits
- Cost savings of $10.30 per patient per month
- Improvements for patients with depression and diabetes
Improving Patient Outcomes
Chronic health conditions require a different care model than acute health conditions. Consistent and timely care of a chronic condition can save your patients time, money, and can add years to their life. By helping your patients effectively manage their chronic health conditions, they are less likely to suffer from other illnesses and injuries.
In addition, properly managing chronic health conditions can lead to an improved quality of life for your patients. They may see improvements in other areas of their life like staying more active, losing weight, and feeling better mentally.
In a recent analysis, patients participating in a structured medically supervised weight management program with RPM lost more than 86% more weight than patients participating in the same program without RPM over 12 weeks. In addition, program completion was more than 30% greater amongst patients participating in RPM.
Today’s Patients Prefer RPM
Patients desire RPM because of the convenience it provides. They can access treatment from the comfort of their homes while avoiding the commute to the physician’s office. RPM allows physicians to monitor and review a patient’s physiological data and health in real-time eliminating the need for patients to keep a written record of their vitals.
Importantly, to deliver the best-in-class RPM services to your patients and receive maximum reimbursements, you must offer cutting-edge remote patient monitoring solutions. Patients will interact directly with the RPM technology you select and therefore you must ensure the product is user-friendly. Patients will consistently use only world-class software and mobile apps.
Takeaways
Remote Patient Monitoring is a broadly accepted treatment protocol that has been proven to increase revenue significantly for practices and simultaneously create substantial efficiencies. In addition, RPM is improving patient care by reducing emergency room visits, hospital admissions and by increasing both the quality and length of life for patients. RPM is an exciting new option for practitioners providing a range of compelling benefits.
For more information about the benefits of RPM, please visit:
Section 3: Remote Patient Monitoring Expands the Potential of Telehealth
CMS has Expanded the Potential of Telehealth
Remote Patient Monitoring makes the remote treatment of patients possible. In addition to telehealth consultations, physicians can now gather real-time vitals from patients and can do so preventatively instead of uncovering a problem months or years after it first presents.
The Centers for Medicare & Medicaid Services (CMS) approved reimbursement for RPM in 2019, defining RPM as:
‘‘The collection of physiologic data (for example, ECG, blood pressure, glucose monitoring) digitally stored and/or transmitted by the patient or caregiver or both to the home health agency.’’
CMS created new CPT codes, as described below, for RPM: 99453, 99454, 99457, 99458 providing for reimbursement of the various components of RPM, including the provision of a device and software, the monitoring of patient data and interactions between patients and their providers.
In 2021, CMS clarified several questions about RPM, including:
- Clarified that after the COVID-19 PHE ends, there must be an established patient-physician relationship for RPM services to be furnished
- Consent to receive RPM services may be obtained at the time that RPM services are furnished
- Junior staff and outside contractors may provide RPM services incident to the billing practitioner’s services and under their supervision
- Clarified that the medical device supplied to a patient as part of RPM services must be a medical device cleared by the FDA
- Clarified that only physicians and NPPs who are eligible to furnish E/M services may bill RPM services
How to Interpret the CMS Definition
CMS has long monitored the value of capturing patient data remotely. The 99091 CPT code has been available to providers for separate reimbursement since 2018, and the code itself has been a valid code since 2002. While this code presented challenges to providers—it was not billable alongside other services and the reimbursement was not significant—it was used and resulted in CMS gathering a great deal of data on the value of monitoring patient data.
In addition, the tremendous costs of emergency room visits and chronic conditions, both in terms of patient mortality and quality of life and actual costs of ongoing and progressively more serious medical care, have convinced CMS of the need to cover services that address these issues.
CMS has included in its description of RPM coverage for the monitoring of many metrics that assist providers in treating patients for a range of conditions, including:
- Obesity
- Hypertension
- Pre-diabetes & Diabetes
- COPD
- Sleep Apnea
- Prenatal and postpartum care
- Pulmonary conditions
See here for a discussion of the top 3 conditions for RPM and here for the specific CPT codes and requirements for billing.
The Difference Between Remote Patient Monitoring and Remote Therapeutic Monitoring
Due to the success of Remote Patient Monitoring, CMS has expanded similar services to other specialities under a new set of codes known as Remote Therapeutic Monitoring. There are key differences between RPM and RTM, including who can bill, the conditions covered and the devices used. See below for a comparison of RPM and RTM.
Section 4: Remote Patient Monitoring Reimbursement
CMS has established CPT codes specific to Remote Patient Monitoring. Importantly, the codes are unbundled and can be billed in addition to E/M codes currently being billed by providers. CMS leverages Current Procedural Terminology (CPT) codes to ensure that healthcare providers capture patient data precisely and submit accurate claims for medical services rendered to Medicare and Medicaid beneficiaries.
What Are CPT Codes?
CPT is a uniform coding system for reporting and describing medical services and procedures. The CPT coding system is created and managed by the American Medical Association (AMA). Depending on their category, CPT codes comprise five characters that are either numeric or alphanumeric:
- Category I CPT Codes: 00100-99499
- Category II CPT Codes: 0001F-9007F
- Category III CPT Codes: 0016T-0207T
How Are CPT Codes Used?
Qualified healthcare professionals (QHPs) in all states use CPT codes to record and describe surgical, medical, evaluation and management, anesthesiology, laboratory, genomic sequencing, and radiology services offered to patients. Physicians send documentation that includes diagnoses codes and CPT codes to federal or private health insurance carriers for reimbursement.
As a physician or QHP, you must have sufficient knowledge of the CPT coding system, so you can bill CMS accurately and get paid correctly and on time. This is especially true if you’re offering RPM services in your practice or have an RPM system in the works.
For more information about CPT Codes:
Remote Patient Monitoring CPT Codes
In 2018, CMS introduced CPT codes to reimburse healthcare practitioners for providing RPM services. You must be well-acquainted and up-to-date with the billing requirements of each RPM CPT code to avoid compensation challenges with CMS. Below the RPM CPT codes you need to know are detailed.
CPT Code 99453
Code 99453 covers the one-time cost of setting up RPM devices and onboarding a patient in your remote healthcare monitoring system. You should bill for CPT 99453 once per patient when starting services.
Billing requirements:
- You must collect a patient’s physiologic data for 16 days during the 30-day billing period
- During the COVID-19 PHE period, you can bill for code 99453 with less than 16 days worth of data for a COVID-related RPM service
- You must use an RPM device that meets the FDA’s description of a medical device
- The RPM treatment must be ordered by a physician or QHP
- Auxiliary personnel (including those “not clinical staff” but employees or leased or contracted employees) are allowed to furnish services under the general supervision of the billing physician or QHP
- The reimbursement rate is $19.73 for both facility and non-facility.*
CPT Code 99454
Code 99454 reimburses you for supplying patients with home health monitoring devices and programming the devices to record physiologic data. You should bill for 99454 once per patient in a 30-day billing period.
Billing requirements:
- You must have 16 days of physiological data and/or alerts during a 30 day period
- During the COVID-19 PHE period, you can bill for code 99454 with less than 16 days worth of data for a COVID related RPM service
- You must dispense the RPM devices for your patients without additional cost to the patient
- You cannot allow patients to bring their own devices or allow leasing of the devices.
- The supplied home monitoring devices must fit the FDA’s description of a medical device
- Even if you issue multiple RPM devices to one patient, you can only bill for code 99454 once in 30 days for all the services
- The RPM device must be ordered by a physician or QHP
- Auxiliary personnel (including those “not clinical staff” but employees or leased or contracted employees) are allowed to furnish services under the general supervision of the billing physician or QHP
- The reimbursement rate is $43.02 for both facility and non-facility.*
CPT Code 99457
Code 99457 reimburses you for the time you spend monitoring, interpreting, and reviewing a patient’s physiological data remotely. You should bill for 99457 once in each calendar month.
Billing requirements:
- You must provide remote health monitoring services for at least 20 minutes per month
- One live interaction is required. CMS calls this an “interactive communication” and defines the interaction as a “ real-time two-way remote communication via video, text, email, phone call, and other virtual interactions between you and your patients”.
- You must be able to furnish CMS with a patient’s treatment plan and recent data outlining beneficiary encounters, when requested
- Services must be performed by QHPs who are eligible to furnish evaluation and management, or auxiliary personnel/clinical staff under the general supervision of the billing provider
- A live interaction cannot be text or email. It must be a live video, phone call, or face-to-face conversation.
- The reimbursement rate is $47.87 for non-facility and $31.15 for facility.*
CPT Code 99458
Code 99458 is an add-on code to 99457 and covers each additional 20 minutes of monitoring. CMS allows up to three units in a calendar month, based on medical necessity.
Billing requirements:
- You can only bill for 99458 as an add-on to code 99457, not as an independent code.
- Services must be performed by QHPs who are eligible to furnish evaluation and management, or auxiliary personnel/clinical staff under the general supervision of the billing provider.
- The reimbursement rate is $38.49 for non-facility and $31.15 for facility.*
The 20 minutes required to bill for 99457 and 99458 includes the time used to set up RPM devices and the time used for interactive communication.
* These are average Medicare rates. Actual reimbursement varies by MAC locality. Private payers set their own rates and are not required to reimburse at the rates set by Medicare.
Section 5: How RPM Reimbursements Work
You must comply with CMS billing rules in order to receive compensation for the remote healthcare monitoring services you offer patients. RPM compensation rates may vary among private insurance companies. However, their figures are typically based on the prevailing rates set by CMS. When reimbursement figures change upon review, CMS publishes the new rates in their annual Physician Fee Schedule report.
Your Revenue Potential from RPM
The better practices do financially, the more they can invest in patient care. Remote Patient Monitoring presents one of the greatest new revenue sources for existing practices.
To review, in summary, the reimbursement for RPM:
- CPT 99453: $19.73 one time
- CPT 99454: $43.02 every month (for passive data collection)
- CPT 99457: $47.87 every month (if actively monitored)
- CPT 99458: $38.49 every month (if actively monitored)
- CPT 99458 (2): $38.49 every month (if actively monitored)
This equates to a minimum revenue of $43.02 every month for every patient you enroll into an RPM program. This minimum reimbursement requires no staff time and is intended to compensate you for the passive collection of data.
Maximum reimbursement is $196.44. To receive the maximum reimbursement, clinical staff must actively monitor and conduct at least one consultation with the patient, spending a total of 60 minutes during the calendar month.
RPM codes are unbundled, which means they do not replace or prohibit practices from billing for other services such as telehealth and chronic care management.
Typical smaller practices generate $250,000 of new annual revenue through RPM. Larger physician groups and health systems can expect $1,000,000 or more in new revenue.
Section 6: Tips for Facilitating CMS Compliance in Your Practice
Outsource Tasks
A good rule of thumb is to outsource your RPM administrative tasks to your RPM platform provider.
These are duties such as documenting your patients’ data, obtaining patient consent, setting up and onboarding patients and staff on your remote health monitoring system, and supplying RPM devices to your patients.
Choose the Right RPM Devices
You must ensure that your patients have a smooth user experience with their wearable health monitoring devices. This way, patients can easily transmit physiological data with minimum downtimes. As a result, you’ll have the required data to bill for codes 99453 and 99454. Devices used for RPM must be FDA medical grade, not consumer grade.
For more information about device options for RPM, please see this detailed review.
Target the Right Patients
Patients with acute conditions, as well as those with chronic conditions such as diabetes, heart disease, and hypertension, benefit most from remote patient monitoring services since they provide an opportunity to collect physiological data daily. You should train such patients to use their RPM devices to collect and transmit data effectively. This will allow you to monitor their health remotely and collect sufficient data to satisfy billing requirements.
It is also important to ensure that you understand insurance coverage for each patient and it is a best practice to complete a benefits eligibility check prior to prescribing RPM.
Section 7: Getting Started with RPM
Implementing Remote Patient Monitoring may seem like a major undertaking for your practice. The reality is that an RPM implementation, with a vendor that is experienced in this area, requires only 3-4 weeks and less than 6 hours of staff time.
The process of implementing a new RPM includes the following:
- Select a vendor
- Set up accounts for providers
- Develop patient identification procedure
- Develop patient script
- Train clinical staff
- Train billing staff
Check out an example of an implementation plan here.
Selecting a Vendor
It is critical to select the right RPM vendor for your practice. There are many reputable RPM vendors available; unfortunately there are also many newly-launched vendors that have little experience. At a minimum, an RPM vendor should:
- Have at least five years of experience in remote monitoring
- Have at least 100,000 patients using the platform
- Be able to provide 6 or more testimonials and referrals
- Provide free and full access to the platform for you to test
- Provide live training for your staff
- Be able to answer any and all of your questions in detail
- Have coding and billing experts on staff and available to you
- Have expertise in practice workflow management
RPM Devices
In order to appropriately deliver and bill for RPM, the devices placed in the patient’s home must be medical-grade, cleared by the FDA and must be provided by the prescribing physician. Patients are not allowed to use their own devices.
Make sure that your RPM vendor provides fully integrated devices and does not use off-the-shelf products (such as FitBit). Your RPM vendor should not only provide devices, but should be experts in how the devices are manufactured. You should avoid RPM vendors that simply buy devices from other companies. This is important due to the complexities of these devices and the enormous importance of providing both reliable devices and expert technical support to patients. Off the shelf devices are typically not developed for the specific RPM use case and this often leads to unreliable data and a lack of patient compliance. The wrong devices will kill your RPM program (or prevent it from ever getting off the ground).
Consider the different connectivity options for devices. There are three options for device connectivity: (1) Bluetooth, (2) cellular, and (3) base station.
Bluetooth
Bluetooth devices connect directly to a mobile app installed on a patient’s phone. This is always the simplest option for patients because there is effectively no set up; these devices work right out of the box and automatically connect to the mobile app without any pairing or syncing necessary. It is important that patients are able to set up their devices easily or they will never engage with RPM.
Bluetooth devices are also the least costly option because they do not have SIM cards like cellular devices or additional hardware like base stations.
The primary drawback to Bluetooth is that patients need to interact with their mobile app and the device to track a measurement whereas cellular and base station options only require patients to interact with their device. There is a silver lining, though. Since patients are engaging with their mobile app each time they record a measurement, typically patients are more engaged overall and share more data, such as meal logging, medication compliance, and other similar metrics.
It is important to note that concerns regarding your patients’ access to a smart phone or the capability to use their smartphone are generally overblown. Even looking at the oldest demographic, these patients are typically using multiple apps, such as video apps to connect with family. Providers report that only approximately 5% of patients are unable to use this technology.
Cellular
Cellular devices are the same as other devices with one difference: they include a SIM card that transmits data automatically over cellular networks. This makes ongoing usage very simple. Patients use the device and the data is sent automatically.
There are two main drawbacks to cellular. First, these options are much more expensive than BlueTooth devices. Initial cost is higher because of the addition of a SIM card, and they require ongoing cellular data plans. Typically, cellular devices cost at least 2x or 3x more than Bluetooth devices initially and several dollars per month in data charges. Second, they are much more difficult to set up initially. This leads to some patients never getting started with RPM and major lost revenue opportunities.
Base Station
Base station is the most complicated and costly option, but it does provide several unique benefits. Base stations use a tracking device, such as a blood pressure cuff, paired to a piece of hardware installed in the home similar to a modem (the base station). The device connects to the base station and the base station sends data automatically.
Usually the base station itself costs multiples of the actual monitoring devices. The primary application for base stations includes very old patients and very sick patients needing multiple devices.
To learn more about RPM devices, please see this informative article:
Rpm Devices: Why Remote Monitoring Technology Should Be Part Of Everyday Healthcare
Section 8: How to Get the Most Out of Your RPM System
Undertaking the implementation of an RPM program is exciting and, when done right, will have a dramatic change on your practice and your patients. Making sure you get the most out of your RPM program is not complicated.
Vendor Selection
Of course, selecting the best RPM software/hardware vendor will have a major impact on the success of your program. Please see above for a discussion of what to look for in RPM vendors. It’s valuable to consider what you need in an RPM vendor. Questions to ask yourself before your vendor evaluations include:
- Is a general RPM platform or one created specifically for my speciality better for me?
- Will I do the monitoring or will I outsource that to my RPM vendor?
- How much support do I need for claims/billing?
- What are the technology needs for my patients?
Asking yourself the right questions upfront will help you better evaluate RPM vendors and avoid being sold on a platform that isn’t right for your practice.
Launch Plan
Creating a strategic launch plan drives a smooth rollout and rapid ramp up of patients into the RPM program. The launch plan should be developed with your RPM vendor (it is a red flag if your RPM vendor does not have a launch plan they have developed based on experience across many implementations). Included in the launch plan should be at least an implementation schedule (training, collateral, approvals, launch date), a standard process for identifying eligible patients, a script for talking to patients and the identification of individuals on the implementation team responsible for various aspects of the process.
Your Responsibilities
In addition to selecting the right vendor, your practice will be instrumental in ensuring the success of your new RPM program. Implementation is a collaborative effort and the following three components are required to ensure a successful RPM launch:
- Leadership from the head of the practice or department to make RPM a core part of patient care
- A point person at the practice responsible for implementation
- Standard operating procedure for identifying eligible patients and ensuring RPM is presented to those patients
Takeaways
With the right vendor, the right launch plan and your collaboration, RPM programs will be highly successful.
If you are not ready to commit to RPM, then wait. There’s no rush and it’s better to wait until you and your practice are ready than to implement now with a lower probability of success.
Section 9: How to Maximize Outcomes
RPM is an opportunity to dramatically impact the quality of care you provide and the medical outcomes your patients experience. RPM enables a paradigm shift from the legacy treatment approach of providing care episodically to providing proactive care based on patient need. The preventative benefits and ability to catch developing problems immediately drive patient health.
Maximizing outcomes for patients requires utilizing RPM programs in the right manner and letting the software support your staff.
Think About Enrollment at the Population Level
Initially, it is valuable to enroll as many patients as are eligible and need the monitoring service. Making a population-level impact requires a meaningful percentage of the population actively participating. Capturing data on the greatest number of patients allows you to triage more effectively and this has the additional benefit of maximizing your revenue.
Utilize the Power of Alerts & Escalation
Setting up your alerts and escalation procedures thoughtfully is how you identify patients in real-time that need your help. This is how you make the best use of a lot of data. The software will crunch all the data for you and then highlight which patients need an intervention. This allows you to treat a developing condition immediately instead of a year later when the patient schedules an annual physical.
Intervene Early & with Precision
Lastly, you will intervene when necessary and target the intervention on the patient’s need. When you are alerted to a patient in need of help, you can take immediate action. You can first review all the data available to you and either make a treatment decision immediately (such as adjusting medication) or schedule a consultation with the patient. Often, you can identify the issue before you speak with the patient and in those cases, you are able to quickly and easily explain the issue and the solution to the patient.
Takeaways
Patient care across your population can be most effectively impacted by implementing RPM with a view towards your entire population vs. individual patients, by utilizing the power of the software to generate alerts and escalations and by intervening with precision.
Section 10: Common RPM Mistakes and How to Avoid Them
It is just as important to implement strategically as described above as it is to avoid common mistakes. Providers have already made mistakes and you can benefit from those experiences by avoiding similar missteps. Some common mistakes include:
Choosing the Wrong Vendor
Choosing the wrong vendor is the most common and most costly mistake. Earlier we described several characteristics to look for in a vendor. It’s also helpful to review red flags that should make you pause and question a potential vendor. Those considerations include:
- Avoid choosing a vendor that has an operating history of fewer than five years or fewer than 100,000 patients. A product that has not been exhaustively tested over many years and a lot of patients will have bugs and problems. Pick and established vendor to avoid being the test case.
- Beware of technology that looks old or dated. If the website or the product itself are poorly designed, the product is likely difficult to use.
- Be sure to talk with someone other than a slick salesperson. Salespeople are paid to get you to sign up even if the product isn’t a good fit. Make sure you speak with the account managers, billing experts, and other support staff. These are the people who actually make your RPM program work.
- Be careful with vendors that do not have deep knowledge of the CPT codes and the billing process. Technology is only one key to success in RPM and vendors that give you a login and walk away aren’t going to be there to support you.
Lacking Commitment
While the salespeople referenced above will tell you to buy an RPM system now, don’t buy it until you’re ready to make RPM a priority in your practice. All staff need to be aligned and understand that RPM will be central to patient care. Lack of commitment to RPM usually results in wasted time and money.
Losing Out on Reimbursements
Certain CPT codes require a certain amount of time to be spent. Make sure staff are hitting that minimum time requirement so you don’t leave money on the table. The best RPM software will track time spent and alert you to patients that are not billable so that you may meet the requirements before the end of the month.
Make sure your billing team is educated on RPM codes and documentation requirements. Address any denials thoughtfully by reviewing the explanation of benefits and the payors policies. Often, a minor change such as adding a diagnosis code will result in payment of the claim.
This guide has been prepared by CoachCare, a leading provider of Remote Patient Monitoring software, devices and service.
This article describes a feature used with the Remote Patient Monitoring (RPM) feature. The information and opinions contained herein are for general information purposes only, are not intended to constitute legal or other professional advice and should not be relied upon nor treated as a substitute for specific advice relevant to particular circumstances. We make no warranties, representations or undertakings about any of the content of this guide (including, without limitation, any as to the quality, accuracy, completeness or fitness for any particular purpose of such content), or any content referred to herein. We make no representations, warranties or guarantees, whether express or implied, that the content of this guide is accurate, complete or up-to-date.